Libido, commonly referred to as sexual desire, is an essential aspect of human life that influences not only intimate relationships but also overall well-being and quality of life. It is a complex interplay of biological, psychological, and social factors that can fluctuate throughout a person’s life. Recognizing and understanding the elements that affect libido can empower individuals to address concerns proactively and foster healthier relationships.
Recent research highlights the prevalence of libido-related issues across various demographics. For example, a study in the Journal of Sexual Medicine reported that approximately 32% of women and 15% of men experience low sexual desire at some point in their lives[1]. These figures emphasize the importance of open dialogue and informed approaches to sexual health.
Factors Influencing Libido

Libido is not a fixed attribute; it is dynamic and can be influenced by a multitude of factors that either enhance or diminish sexual desire. Understanding these factors is crucial for addressing any concerns related to sexual health.
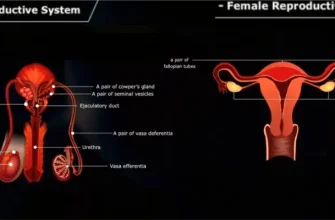
Biological Factors
Biological components play a significant role in shaping an individual’s libido. Hormones, neurotransmitters, and overall physical health are key contributors.
Hormonal Fluctuations are perhaps the most influential biological factor. In men, testosterone is the primary hormone driving sexual desire. Low levels of testosterone can lead to a decreased libido, fatigue, and mood disturbances[2]. In women, estrogen and progesterone levels fluctuate during menstrual cycles, pregnancy, and menopause, affecting sexual desire and arousal. For instance, during menopause, the decrease in estrogen can lead to vaginal dryness and discomfort during intercourse, potentially reducing libido[3].
Neurotransmitters in the brain, such as dopamine and serotonin, also influence sexual desire. Dopamine is associated with pleasure and reward, enhancing libido, while serotonin can have inhibitory effects on sexual function. Medications like selective serotonin reuptake inhibitors (SSRIs), commonly used as antidepressants, can increase serotonin levels and may inadvertently reduce sexual interest and performance[4].
Medical Conditions can have a profound impact on sexual desire. Chronic illnesses like diabetes, hypertension, and cardiovascular diseases can impair blood flow and nerve function, leading to difficulties in sexual performance and reduced libido[5]. Additionally, medications used to treat these conditions may have side effects that negatively affect sexual desire.
Psychological Factors
The mind plays an integral role in sexual desire. Psychological well-being can either enhance or inhibit libido.
Stress and Anxiety are common psychological factors that can suppress sexual desire. High levels of stress increase the production of cortisol, a hormone that can interfere with sex hormones and reduce libido[6]. Anxiety about sexual performance, work pressures, or financial concerns can distract individuals from sexual intimacy.
Depression often diminishes interest in activities that were once pleasurable, including sex. The emotional numbness and fatigue associated with depression can lead to a significant decrease in libido[7]. Furthermore, some antidepressant medications can exacerbate this issue due to their impact on neurotransmitters.
Self-Esteem and Body Image influence how comfortable individuals feel about engaging in sexual activity. Negative perceptions of one’s body can lead to self-consciousness, reducing sexual confidence and desire. On the other hand, a positive body image can enhance libido by increasing comfort and openness during intimate moments.
Social and Relationship Factors
The context of relationships and societal influences significantly affect libido.
Relationship Satisfaction is directly correlated with sexual desire. Open communication, emotional intimacy, and mutual respect foster a healthy sexual relationship. Conversely, unresolved conflicts, lack of trust, or poor communication can lead to decreased libido[8]. Partners who feel emotionally disconnected may find their sexual desire waning.
Cultural and Religious Beliefs shape attitudes toward sex and can either encourage or inhibit sexual expression. Societal norms may place taboos on discussing sexual desires, leading to suppression of libido. Religious teachings may also influence how individuals perceive sex, potentially causing internal conflicts that affect desire.
Life Transitions such as childbirth, career changes, or the loss of a loved one can temporarily affect libido. These events often require significant emotional and physical adjustments, which can divert energy away from sexual activities.
Libido Across Different Life Stages

Sexual desire evolves throughout an individual’s life, influenced by physiological changes and life experiences.
Adolescence
During puberty, hormonal changes trigger the development of secondary sexual characteristics and the awakening of sexual desire. Teenagers experience new emotions and physical sensations, often accompanied by curiosity and experimentation. Education on sexual health, consent, and emotional readiness is vital at this stage to promote healthy attitudes toward sex.
Adulthood
In early adulthood, individuals often explore their sexual identities and preferences. This period can be marked by strong sexual desire, but it may fluctuate due to stressors such as building careers, financial responsibilities, and forming long-term relationships. A study indicated that over 60% of adults aged 25-45 reported that stress negatively impacts their sexual desire[9].
Midlife and Menopause
As individuals reach midlife, hormonal changes become more pronounced. Women experience menopause, leading to decreased estrogen levels, which can cause vaginal dryness, hot flashes, and reduced libido[3]. Men may experience andropause, characterized by a gradual decline in testosterone levels, potentially leading to decreased sexual desire and energy levels[2]. Addressing these changes openly with partners and healthcare providers can help mitigate their impact.
Senior Years
Sexual desire in older adults varies widely. Many maintain an active sex life, finding intimacy important for emotional connection and quality of life. Physical health issues may arise, but with medical advancements and open communication, many barriers to a satisfying sex life can be overcome. Societal attitudes are gradually shifting to recognize and support the sexuality of older adults.
Common Issues Affecting Libido

Understanding common issues can help in seeking appropriate solutions.
Hypoactive Sexual Desire Disorder (HSDD)
HSDD is characterized by a persistent lack of sexual desire causing significant distress. It affects about 10% of women and a smaller percentage of men[10]. Causes can be multifaceted, including hormonal imbalances, psychological factors, and side effects of medications. Treatment often involves a combination of hormonal therapy, counseling, and lifestyle changes.
Sexual Aversion Disorder
This condition involves an extreme aversion to sexual contact, leading to avoidance of intimacy. It may stem from past traumas, such as sexual abuse, or severe anxiety disorders. Professional psychological intervention is crucial for addressing underlying issues and helping individuals regain comfort with intimacy.
Hypersexuality
An unusually high sex drive can sometimes be symptomatic of underlying conditions.
Manic Episodes in bipolar disorder may involve increased sexual activity and risk-taking behaviors[11]. Recognizing these patterns is important for appropriate mental health treatment.
Compulsive Sexual Behavior may also be associated with neurochemical imbalances or as a coping mechanism for emotional distress. Professional help can assist in managing these behaviors effectively.
Enhancing Libido: Strategies and Solutions

Addressing libido concerns requires a holistic approach that considers physical, emotional, and relational aspects.
Lifestyle Modifications
Implementing positive lifestyle changes can significantly enhance libido.
Nutrition plays a foundational role. Consuming a balanced diet rich in whole foods, lean proteins, healthy fats, and plenty of fruits and vegetables supports overall health and hormonal balance. Certain nutrients, such as zinc and omega-3 fatty acids, are essential for hormone production and can be found in foods like seafood, nuts, and seeds.
Physical Activity enhances blood circulation, boosts energy levels, and promotes the release of endorphins, improving mood and reducing stress[12]. Regular exercise can also improve body image and self-esteem, contributing to increased sexual desire.
Sleep Hygiene is crucial for hormonal regulation and energy. Lack of sleep can lead to fatigue and decreased libido. Establishing a regular sleep schedule and creating a restful environment can improve sleep quality.
Stress Reduction Techniques such as meditation, deep-breathing exercises, yoga, and engaging in hobbies can lower cortisol levels and alleviate stress-induced libido decline.
Medical and Therapeutic Interventions
When lifestyle changes are insufficient, medical and therapeutic interventions may be necessary.
Medical Evaluation by a healthcare professional can identify underlying medical issues contributing to low libido. Hormone replacement therapy might be recommended for individuals with significant hormonal deficiencies[13].
Psychotherapy and Counseling can address psychological barriers. Cognitive-behavioral therapy (CBT) and sex therapy can help individuals and couples work through issues like anxiety, depression, past traumas, and relationship conflicts. Therapists provide strategies to enhance communication, intimacy, and sexual satisfaction.
Medication Review is important, especially if current medications have side effects that impact libido. A healthcare provider may adjust dosages or suggest alternative medications with fewer sexual side effects.
Communication with Partners
Open and honest communication with a partner is essential. Discussing desires, boundaries, and concerns can strengthen the emotional connection and enhance intimacy. Couples may explore new ways to experience pleasure, such as trying different forms of physical affection, scheduling intimate time, or incorporating elements that increase comfort and excitement.
Statistical Insights

Global Prevalence: Sexual dysfunction affects a significant portion of the population, with studies showing prevalence rates of 43% in women and 31% in men for various sexual issues[1].
Impact of Mental Health: Individuals suffering from depression are twice as likely to experience low libido compared to those without depression[7].
Effectiveness of Therapy: Approximately 70% of couples report improved sexual satisfaction after participating in relationship counseling and therapy[14].
Libido and sexual desire are integral components of human health and relationships. They are influenced by a myriad of factors that can change over time. Recognizing and understanding these factors empowers individuals to take proactive steps in addressing concerns.
By embracing a holistic approach that includes lifestyle modifications, medical interventions, and open communication, individuals can enhance their sexual desire and overall satisfaction. It is important to acknowledge that fluctuations in libido are normal and that seeking support from healthcare professionals is a positive step toward well-being.
Creating a culture where discussions about sexual health are normalized can lead to better outcomes and more fulfilling relationships. Education, empathy, and proactive engagement are key to navigating the complexities of libido and desire.
References:
- Laumann, E. O., Paik, A., & Rosen, R. C. (1999). Sexual dysfunction in the United States: prevalence and predictors. JAMA, 281(6), 537-544.
- Mulligan, T., Frick, M. F., Zuraw, Q. C., Stemhagen, A., & McWhirter, C. (2006). Prevalence of hypogonadism in males aged at least 45 years: the HIM study. International Journal of Clinical Practice, 60(7), 762-769.
- Burger, H. G. (2008). The endocrinology of the menopause. Maturitas, 61(1-2), 231-236.
- Clayton, A. H., Warnock, J. K., Kornstein, S. G., Pinkerton, R., Sheldon-Keller, A., & McGarvey, E. L. (2002). A placebo-controlled trial of bupropion SR as an antidote for selective serotonin reuptake inhibitor-induced sexual dysfunction. Journal of Clinical Psychiatry, 63(4), 357-364.
- Nicolosi, A., Moreira, E. D., Shirai, M., Bin Mohd Tambi, M. I., & Glasser, D. B. (2003). Epidemiology of erectile dysfunction in four countries: cross-national study of the prevalence and correlates of erectile dysfunction. Urology, 61(1), 201-206.
- Chrousos, G. P., & Gold, P. W. (1992). The concepts of stress and stress system disorders: overview of physical and behavioral homeostasis. JAMA, 267(9), 1244-1252.
- Kennedy, S. H., Dickens, S. E., Eisfeld, B. S., & Bagby, R. M. (1999). Sexual dysfunction before antidepressant therapy in major depression. Journal of Affective Disorders, 56(2-3), 201-208.
- Mark, K. P., & Murray, S. H. (2012). Gender differences in desire discrepancy as a predictor of sexual and relationship satisfaction in a college sample of heterosexual romantic relationships. Journal of Sex & Marital Therapy, 38(2), 198-215.
- O’Sullivan, L. F., & Brotto, L. A. (2016). A comparison of heterosexual and sexual-minority women’s sexual and relationship satisfaction. Journal of Sex Research, 53(6), 681-696.
- West, S. L., Vinikoor, L. C., & Zolnoun, D. (2004). A systematic review of the literature on female sexual dysfunction prevalence and predictors. Annals of Internal Medicine, 140(6), 1-11.
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
- Stathopulos, A., & Arnold, C. (2013). The effects of physical exercise on female sexual functioning and sexual desire. The Journal of Sexual Medicine, 10(3), 898-899.
- Basson, R., Rees, P., Wang, R., Montejo, A. L., & Incrocci, L. (2010). Sexual function in chronic illness. The Journal of Sexual Medicine, 7(1 Pt 2), 374-388.
- Lebow, J. (2012). Overview of the research on couple and family therapy. Journal of Marital and Family Therapy, 38(1), 145-168.

Emily Dailey
Sexual Wellness Editor
Emily Dailey has over 10 years of experience writing and curating content about sexuality and relationships. With a portfolio of 150+ articles, she is dedicated to promoting open conversations and helping people embrace their desires with confidence and understanding.